“With my case, I want to win a #ITIWS24freeticket to attend the ITI World Symposium 2024 from May 9-11 for free”.
Immediacy is today the driving force in modern implantology. With meticulous case selection, precise choice of implant designs (micro & macro), biomaterials along with the optimally invasive surgical techniques, it can utilized to obtain predictable & stable treatment outcomes. The concept of immediacy brings along host of benefits to both clinician& patient alike.
Case Scenario:
A 53 year old female patient reported to us with gingival recession, mobility with upper left canine, premolars & missing molar teeth and wanted fixed replacement of the same.
Intraoral examination revealed previous endodontic treatment with 23. Old splinted FDPs (24-25) with fractured ceramic facings H\o endodontic treatment. Grade 2-3 mobility was seen with these teeth. She also gave a H\o periodontal therapy around 3-4 years ago. No signs of active infection or sinus tract seen. Teeth 23,24,25 had poor prognosis and were deemed for extractions.
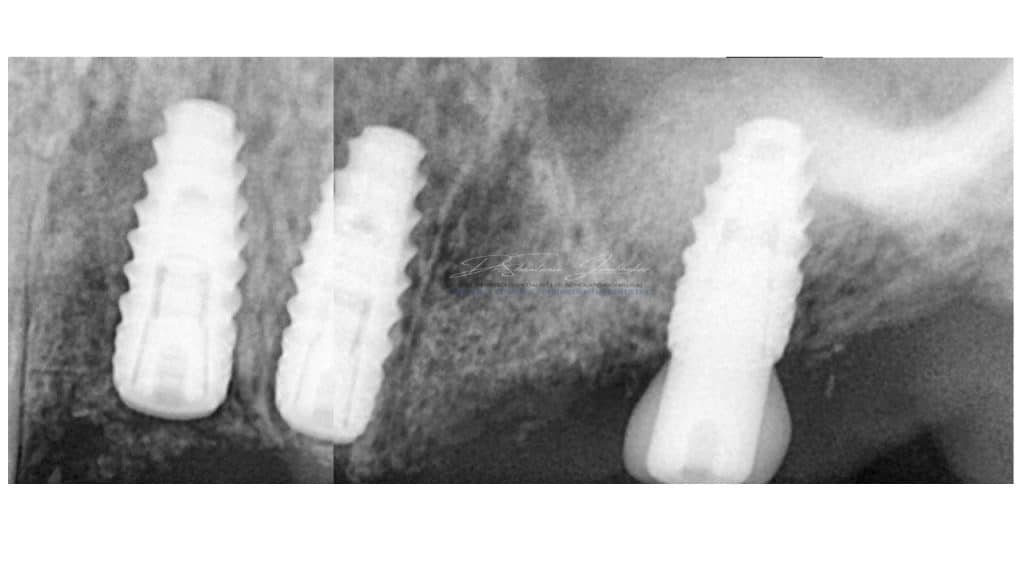
Radiographic examination revealed radiolucent lesion with 23,25 and reduced residual ridge dimensions with sites 26 & 27. Cone beam CT (CBCT) evaluation was performed for available quantity & quality of bone at the proposed implant sites using CS 3D Software.
Treatment Planning & Execution:
Surgical Phase:
Extraction & Immediate Implant (Type I) placements were performed for site 23,24 along with Guided Bone Regeneration using Xenograft from Geistlich BioOss and GBR Membrane along with collagen fleece with two stage protocol (submerged healing with healing screws).
Conelog Progressive line Fixtures were placed 4.3X 9 at both sites. Fixtures were selected based on their variable Implant thread design and fixture morphology with active threads all the way down to the apex which offers excellent primary stability even in deficient bone conditions.
- Implant Site 26& 27#(#27 was optional & patient opted to have it done at later stage)
Minimally Invasive Crestal Approach Sinus Augmentation (MITSA) was performed with Crestal Approach Sinus Kit from Osstem Implants, Korea and sinus augmented with Novabone Putty.
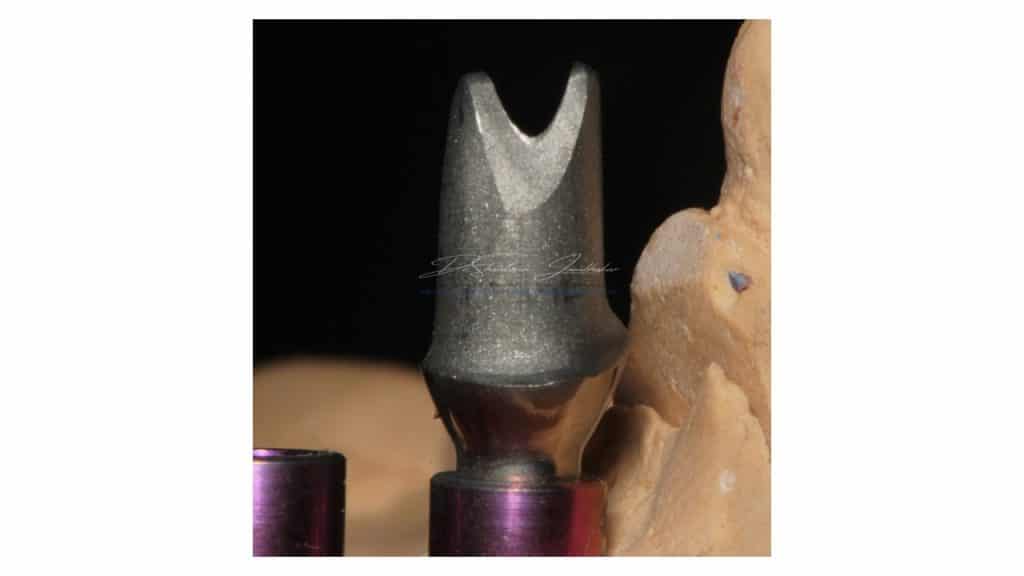
Conelog Progressive Line fixture 4.3X7 was placed along with a Customized Healing abutment to create a wider emergence & prevent fixture to be inadvertently pushed into the sinus. The fixture has crestal anchorage thread design which allows excellent primary stability even in minimally available residual ridge dimensions in the posterior maxillae.
Prosthetic Phase:
Implant Recovery:
Implant recovery and soft tissue modulation was performed using Customized healing abutments and modified incision design to improve the buccal tissue drape around the fixtures.
Prosthetic Design:
23- Cement Retained individual FDP in Monolithic Multilayered Zr using a stock Esthomic abutment.
24-25-26: 3 Unit Screw retained FDP in Monolithic Multilayered Zr using Ti- abutments suited for bridge reconstructions(non-engaging)
Biolase Epic X was utilized for minor frenectomy of the buccal frenii to eliminate the tension on the marginal ginvivae along the buccal aspect of the prosthesis.

Pre-Treatment Baseline

Pre-Treatment IOPA showing the periodontal defect
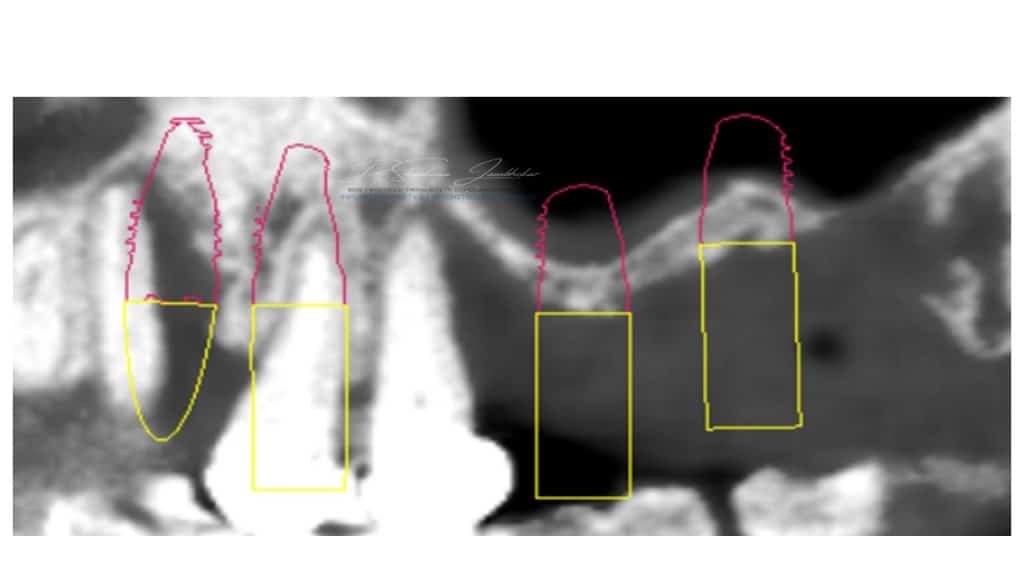
Implant treatment Planning on CS3D software

Minimally Traumatic Extractions
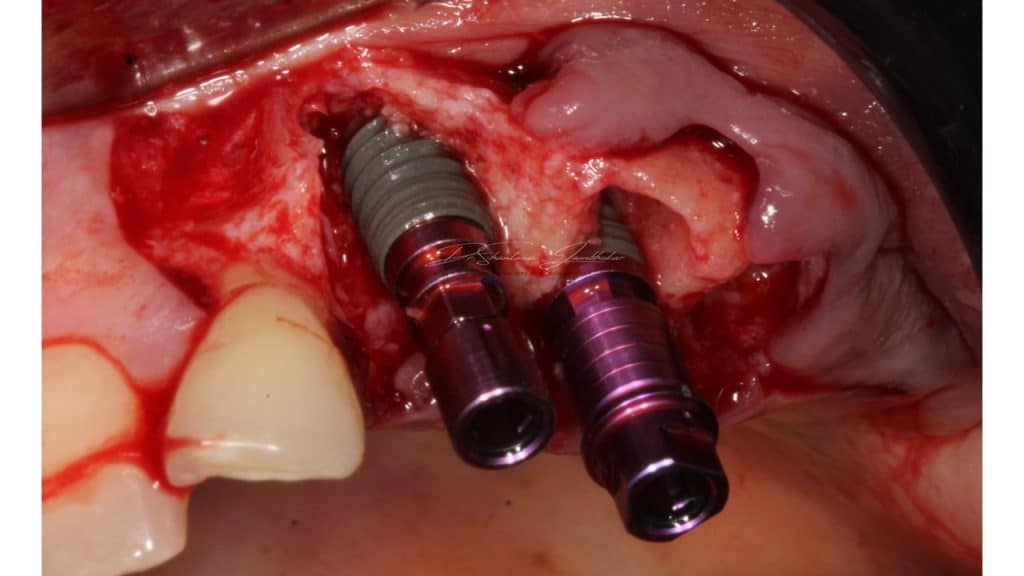
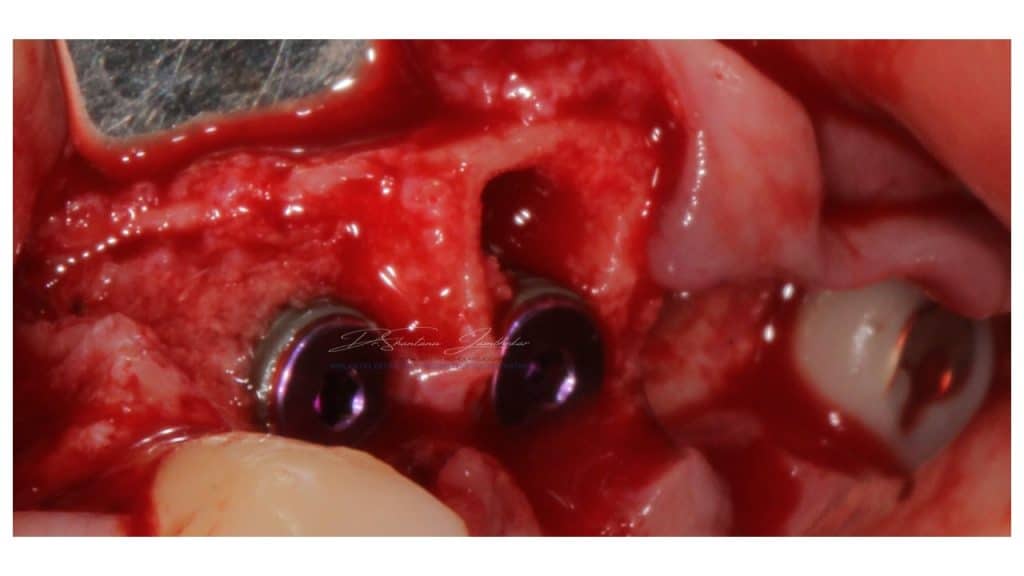
Immediate Implants (Type I) placed with site 23 & 24
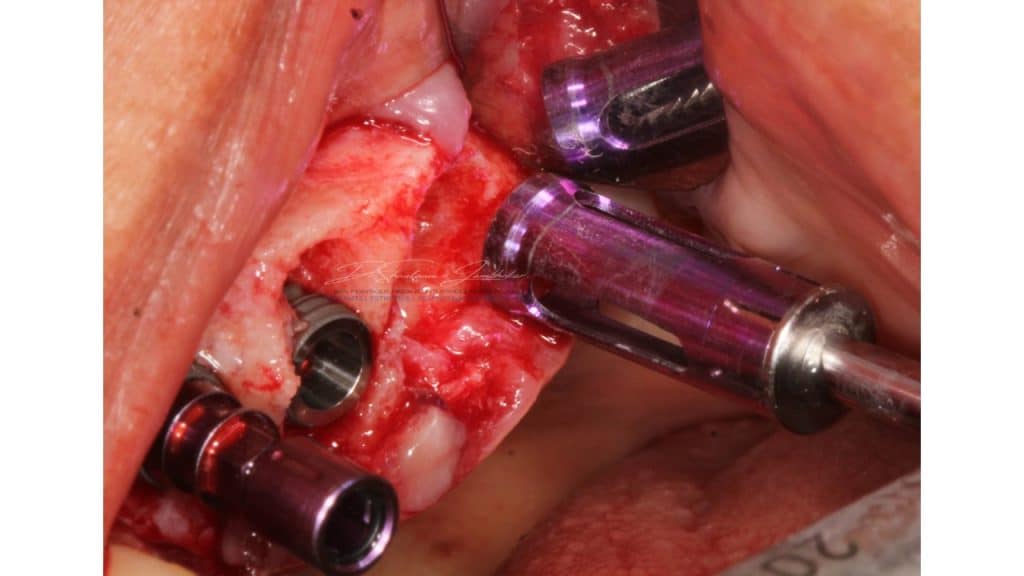
CAS Kit drills with stoppers used to perform the osteotomy

Crestal Approach Sinus Elevation being performed with CAS Kit
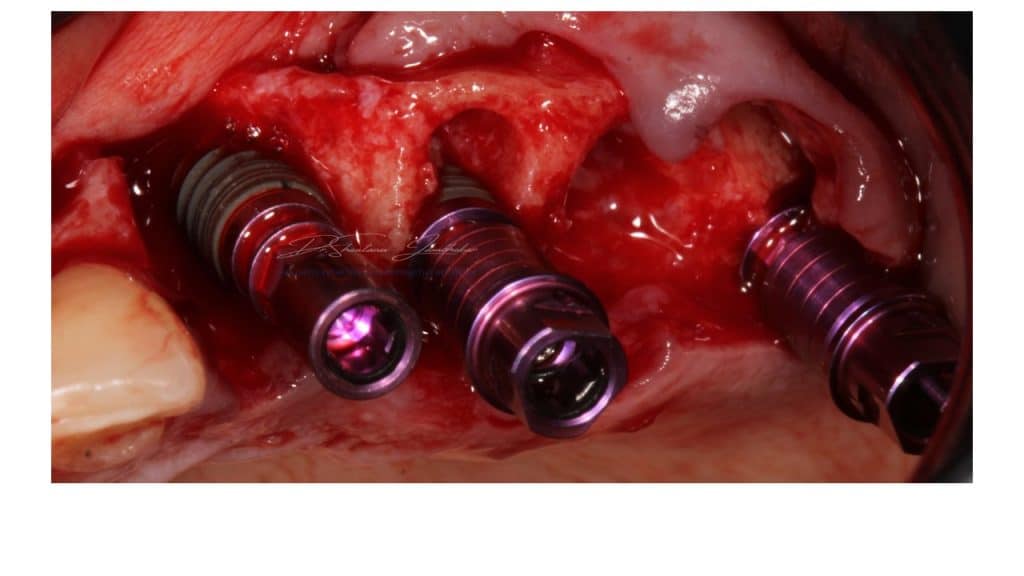
Implants in situ with Mounts in Site 23,24 & 26
Covers screws connected with site 23,24 for closed healing & 26 with wide emergence custom healing abutment
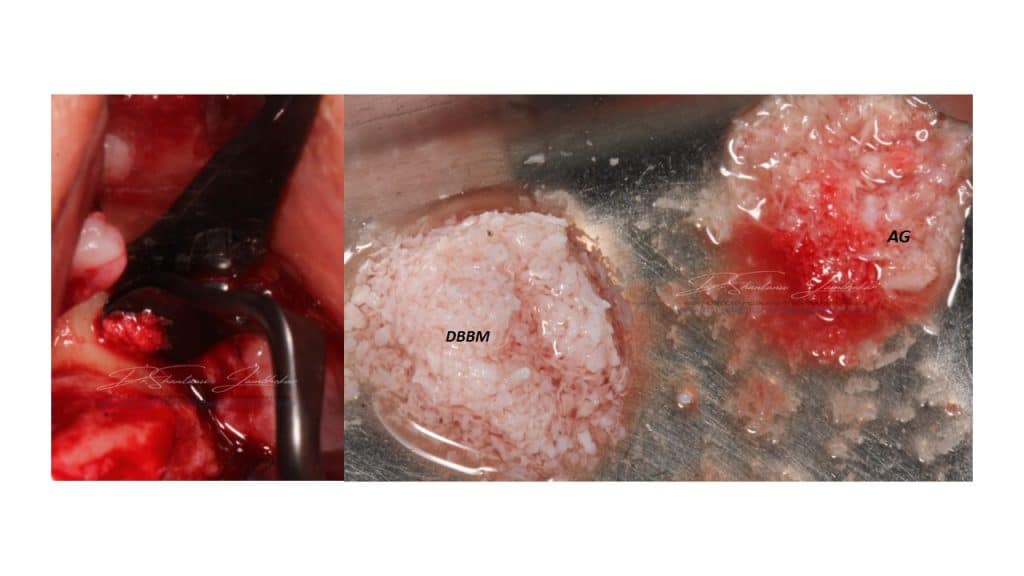
Buser Scrapper from Hu Friedy for harvesting autogenous bone. DBBM (BioOss) and Autogenous bone for GBR
Implant surface covered with autogenous bone scrappings
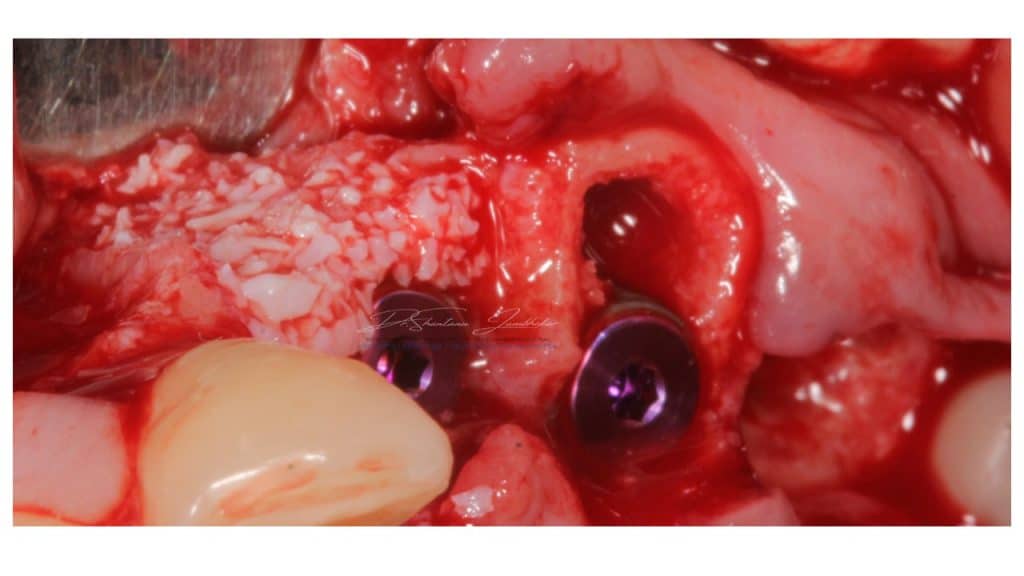
Second layer of Composite(Autogenous+xenograft 50:50 mix) layered
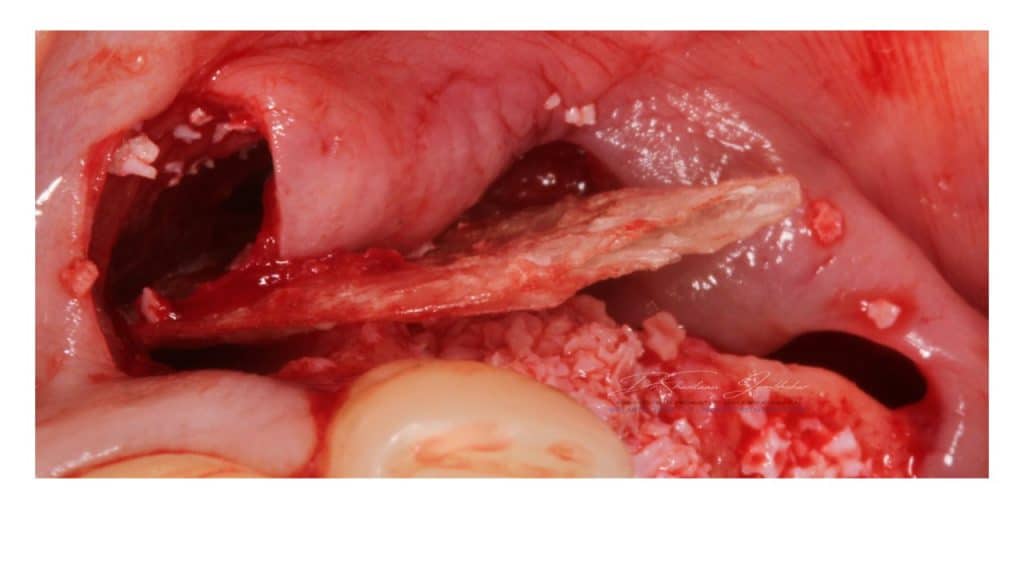
GBR membrane placed

GBR membrane covered with collagen fleece membrane
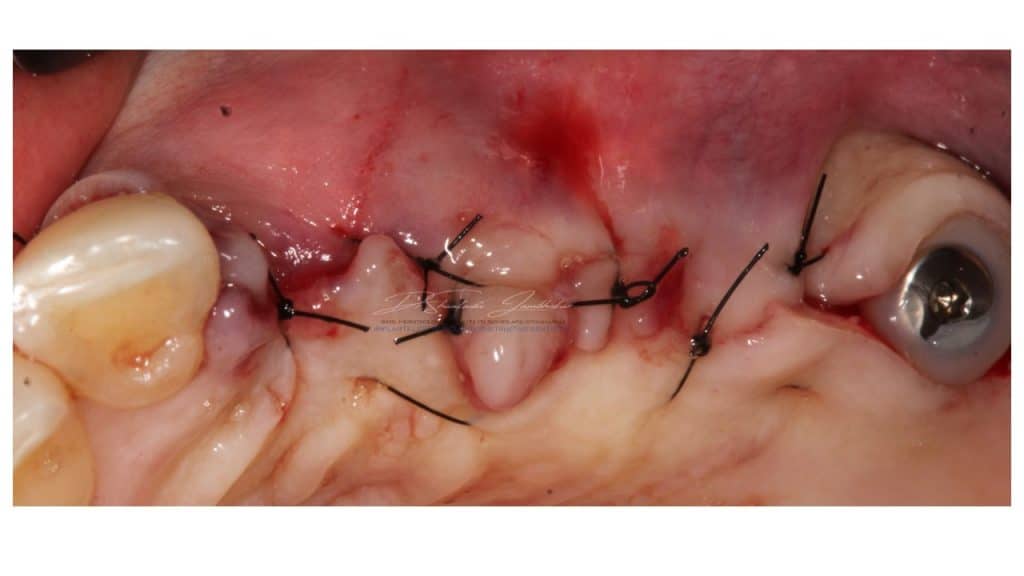
Primary closure with 5-0 Nylon sutures

Post Healing Phase of 6 months
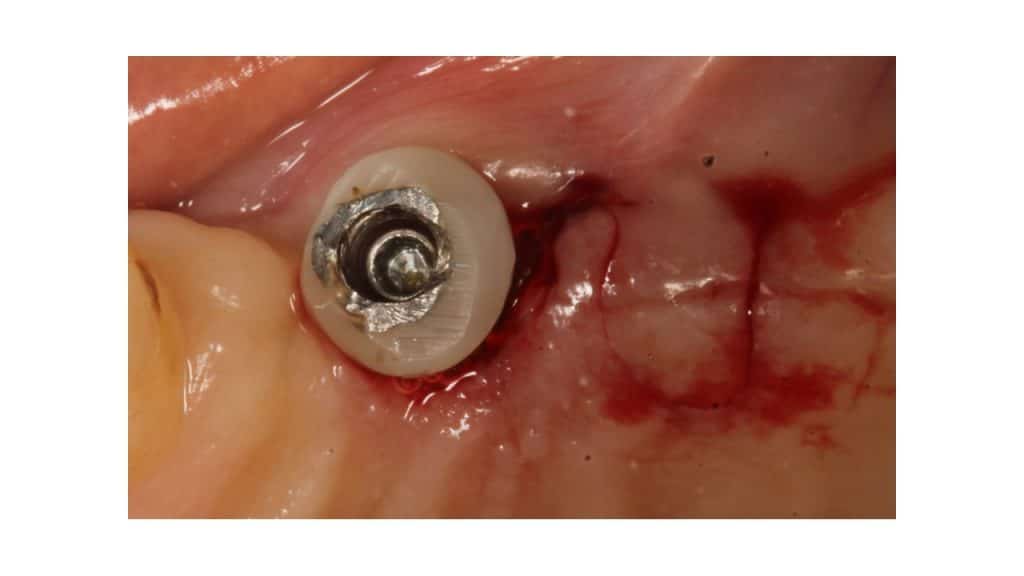
Modified flap design for buccal soft tissue augmentation and custom healing abutment in situ

Post 4 weeks of healing with custom healing abutments
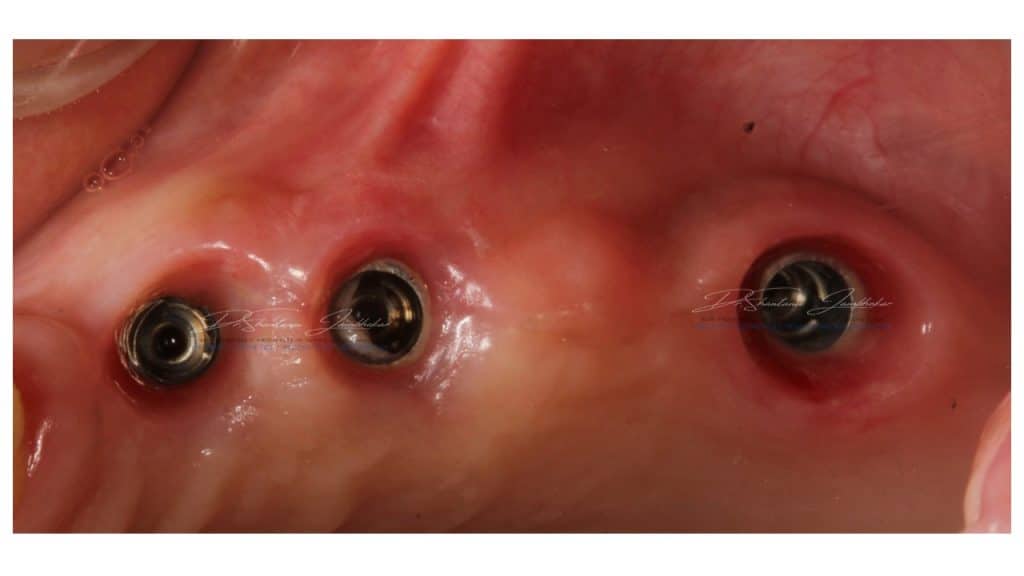
Optimal emergence profiles obtained at 23,24 & 26
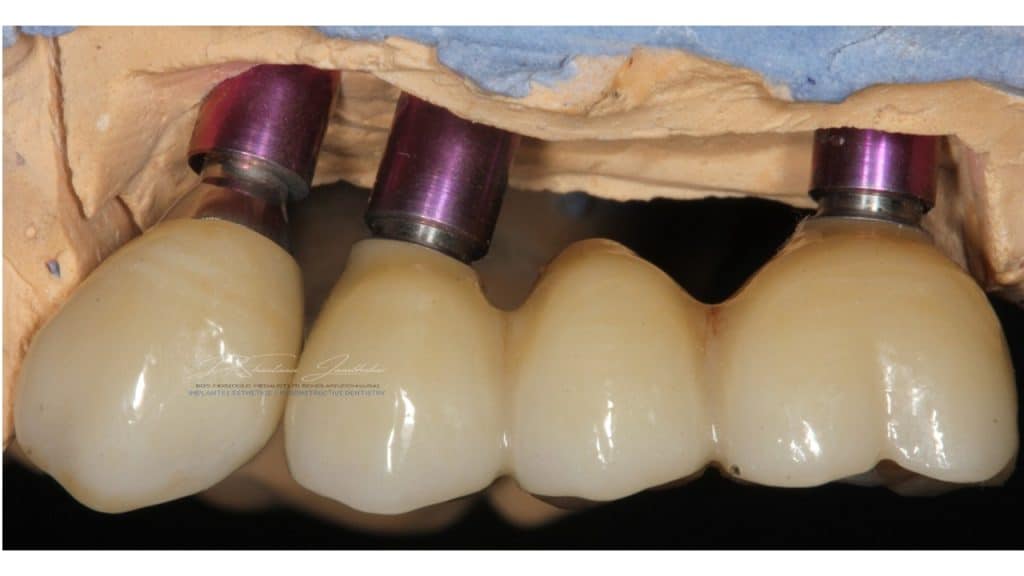
Cement retained Monolithic Zr Implant Restorations with 23 & Screw retained Monolithic Zr Implant restorations using Ti-base abutment with 24-25-26
Esthomic Abutment with 23

Pontic Site modification with site 24 using Biolase Epic X laser

Definitive prosthesis delivered. Buccal freni showing pull\tension on tissues buccal to the prosthesis
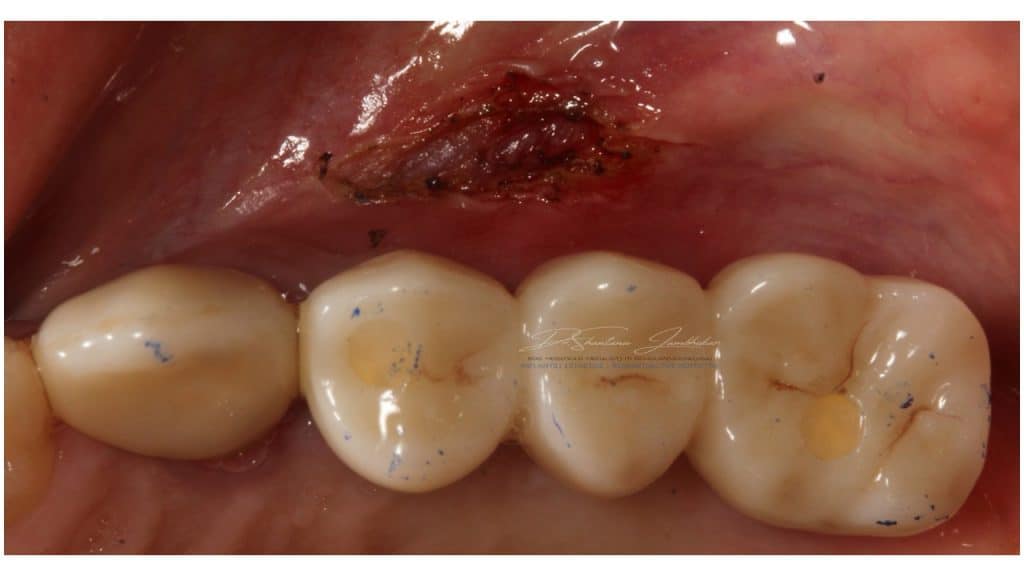
Laser frenectomy

Post treatment at 2 weeks
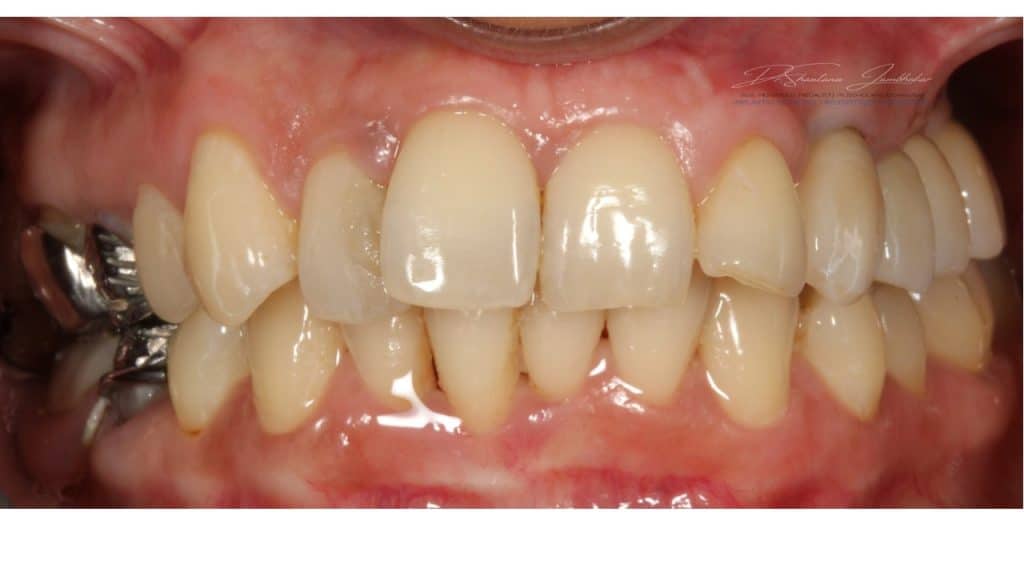
Post treatment image at 12 months followup

Post Treatment Follow up at 22 months

IOPA at 22 month Follow up
Share on:
