Below is a clean, publication-ready Zerodont professional article.
No images referenced. Focused on single-visit endodontics followed by biomimetic composite onlay for a mandibular first molar (lower 6), written in an academic but readable tone.
Single-Visit Endodontic Treatment Followed by Biomimetic Composite Onlay Restoration in a Mandibular First Molar
A restorative-driven endodontic approach
Abstract
The long-term success of endodontic therapy is inseparably linked to the quality and timing of the definitive coronal restoration. This case report describes a single-visit endodontic treatment of a mandibular first molar followed by immediate biomimetic composite onlay restoration under rubber dam isolation. The workflow emphasizes endo-restorography, preservation of tooth structure, immediate coronal sealing, and cuspal coverage using adhesive dentistry principles to restore function, strength, and biological integrity.
Introduction
Mandibular first molars are structurally vulnerable teeth due to their complex root canal anatomy, high occlusal load, and frequent history of extensive caries or restorations. After endodontic treatment, these teeth demonstrate a significantly increased risk of fracture if cuspal protection is delayed or neglected.
Modern restorative dentistry has shifted from post-centric approaches toward adhesive, biomimetic strategies that aim to reinforce remaining tooth structure, reduce flexure, and restore biomechanical behavior close to that of natural teeth. When performed under strict isolation and magnification, single-visit endodontics followed by immediate bonded cuspal coverage can improve prognosis while minimizing contamination and treatment time.
Case Overview
A mandibular first molar (lower 6) presented with deep carious involvement and symptoms consistent with irreversible pulpitis. Radiographic assessment revealed intact periapical structures with no evidence of apical pathology. Given the favorable biological status, a single-visit endodontic and restorative approach was planned.
The treatment objective was not merely canal obturation, but complete endo-restorative integration with immediate coronal sealing and cuspal protection.
Clinical Procedure
Isolation and Access
After anesthesia, the tooth was isolated using a rubber dam to ensure asepsis throughout both endodontic and restorative phases. Access cavity preparation was carried out conservatively, prioritizing preservation of pericervical dentin.
Root Canal Treatment
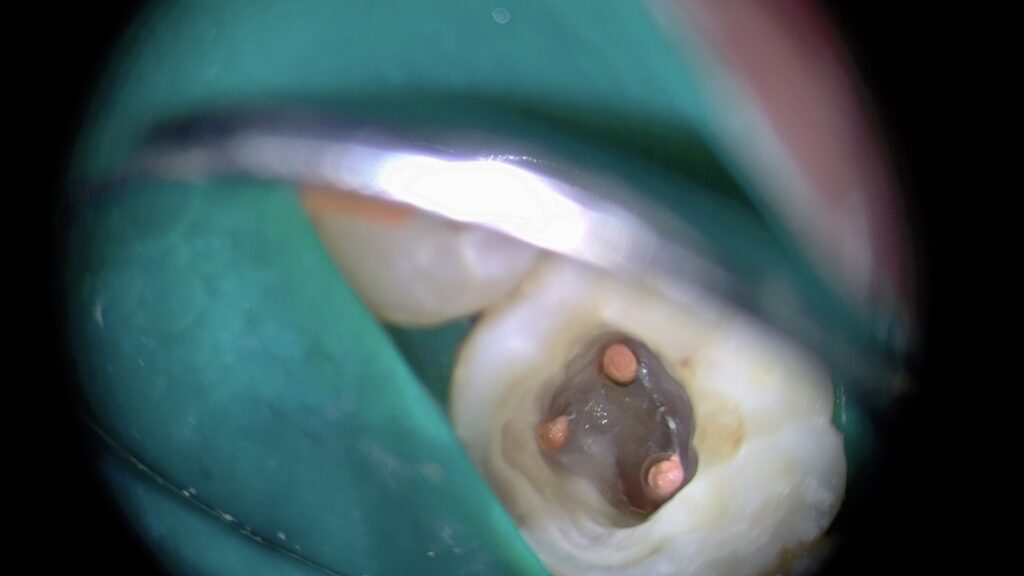
All canals were identified and negotiated under magnification. Cleaning and shaping were performed using a crown-down approach with copious irrigation to ensure effective disinfection while minimizing dentin removal. Canals were obturated in the same visit following confirmation of working length and apical patency.
Immediate placement of a bonded core was performed to prevent coronal leakage and reinforce remaining tooth structure.
Restorative Phase: Biomimetic Composite Onlay
Rationale for Cuspal Coverage
Endodontically treated mandibular molars are subject to cuspal deflection under occlusal forces. In this case, direct cuspal coverage with a bonded composite onlay was selected to:
- Reduce cuspal flexure
- Distribute occlusal stresses
- Avoid unnecessary removal of sound tooth structure
- Provide immediate functional rehabilitation
Adhesive Protocol
The tooth was re-isolated under rubber dam. Enamel margins were refined and selectively etched to maximize enamel bonding while protecting dentin. A multi-step adhesive protocol was used to ensure optimal hybridization and marginal integrity.
Composite Onlay Build-Up
The onlay was built incrementally using a stress-reduced layering technique. Cusps were reconstructed anatomically, respecting occlusal morphology and functional pathways. Occlusion was carefully adjusted to avoid high-stress contacts, particularly in lateral excursions.
Finishing and polishing were performed to achieve smooth margins, proper contact areas, and a natural surface texture.
Outcome and Prognosis
The final restoration provided immediate cuspal protection, an effective coronal seal, and restoration of occlusal function. Radiographic evaluation confirmed dense root canal obturation and proper adaptation of the restorative material.
By integrating endodontic and restorative procedures into a single, well-controlled session, the risk of bacterial recontamination and structural failure was significantly reduced.
Discussion
This case highlights the importance of endo-restorography, where endodontic treatment is planned in direct continuity with the final restoration. Evidence consistently shows that the survival of endodontically treated teeth depends more on the quality of the coronal restoration than on the root canal filling itself.
Biomimetic composite onlays offer a conservative alternative to full-coverage crowns, particularly when enamel margins are preserved and rubber dam isolation is strictly maintained. When combined with immediate restoration, single-visit endodontics can be both biologically sound and mechanically predictable.
Conclusion
Single-visit endodontic treatment followed by immediate biomimetic composite onlay restoration represents a contemporary, evidence-based approach for managing mandibular first molars. By respecting tooth biology, preserving structure, and restoring biomechanics through adhesive dentistry, long-term functional success can be achieved without overtreatment.
References
- Magne P, Belser U. Adhesive restorations, centric relation, and the cracked tooth dilemma. Quintessence Int. 2002.
- Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage. J Prosthet Dent. 2005.
- Tang W, Wu Y, Smales R. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010.
- Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010.
- Ferrari M, et al. Bonding to enamel and dentin: fundamental aspects for clinical success. J Adhes Dent. 2015.
- Rocca G, Krejci I. Bonded indirect restorations for posterior teeth: from cavity preparation to restoration. Int J Esthet Dent. 2015.



{"tiktok_developers_3p_anchor_params":"{"filter_id":[],"template_id":"","capability_key":["edit"],"capability_extra_v2":{"edit":[{"panel":"hd_quality_picture"}]},"client_key":"awgvo7gzpeas2ho6"}","source_type":"hypic","data":{"filterId":"","pictureId":"18E4DF28-5850-4F13-9B7B-D7BEF721EF36","stickerId":"","imageEffectId":"","activityName":"","playId":"","enter_from":"enter_launch","os":"ios","appversion":"8.0.0","infoStickerId":"","product":"retouch"}}

{"source_type":"hypic","tiktok_developers_3p_anchor_params":"{"capability_key":["edit"],"filter_id":[],"template_id":"","client_key":"awgvo7gzpeas2ho6","capability_extra_v2":{"edit":[{"panel":"hd_quality_picture"}]}}","data":{"appversion":"8.0.0","filterId":"","infoStickerId":"","imageEffectId":"","activityName":"","os":"ios","playId":"","stickerId":"","enter_from":"enter_launch","product":"retouch","pictureId":"46756AC5-79CC-40FF-A254-E7EC11D64CF8"}}

{"data":{"filterId":"","infoStickerId":"","os":"ios","enter_from":"enter_launch","playId":"","pictureId":"02FD43A4-BBE4-45B9-9527-969EB5FF4310","activityName":"","product":"retouch","stickerId":"","imageEffectId":"","appversion":"8.0.0"},"source_type":"hypic","tiktok_developers_3p_anchor_params":"{"client_key":"awgvo7gzpeas2ho6","template_id":"","capability_key":["edit"],"capability_extra_v2":{"edit":[{"panel":"hd_quality_picture"}]},"filter_id":[]}"}

Share on:
